2/8/14.....
2/7/14.....
2/6/14.....
2/4/14......
http://www.latimes.com/business/la-fi-obamacare-patients-20140205,0,5417742.story#axzz2sQssirFs
http://www.zerohedge.com/news/2014-02-04/obamacare-crush-workforce-25-million-workers-next-decade-cbo-admits
2/3/14....
KTTC Rochester, Austin, Mason City News, Weather and Sports
http://twitchy.com/2014/02/01/i-will-not-comply-doctor-slams-obamacare-sends-must-read-breakup-letter-to-aetna/
Aetna CEO: Pulling out of ObamaCare is still an option if the program doesn’t “settle down”
POSTED AT 1:01 PM ON FEBRUARY 8, 2014 BY ERIKA JOHNSEN
Last month, Aetna’s CEO Mark Bertolini casually dropped the hint that his insurance company might have to consider ducking out of ObamaCare if the program doesn’t get its act together, especially in terms of providing more certainty for insurers (…the poor dears). That evidently got the administration’s attention, and Bertolini mentioned this week on CNBC that Obama officials have been in contact trying to figure out what it would take to keep Aetna in the system. I’d imagine that one of the biggest trending topics under discussion had to do with the report this week that the Obama administration is considering extending their belated “administrative fix” meant to smooth over their farcical “if you like your plan, you can keep it” lie and millions of Americans’ cancelled policies. In order to avoid pulling out or substantially raising prices, Bertolini mentioned, “We need to understand where we’re headed with any number of programs… are we going to be required to have people keep what they have for another year or more?”
There is so much uncertainty about Obamacare that Aetna, the U.S.’s third-largest insurance provider, may be forced to double its rates or opt out of the program, the company’s CEO, Mark Bertolini, told CNBC on Thursday.What action Aetna will take is still up in the air, but the company doesn’t plan to set its 2015 Obamacare rates until May 15. Between now and then, though, Bertolini said he’s trying to get the necessary information from the Obama administration to properly price its insurance products.“I think in the end analysis, pulling out is always the last resort,” Bertolini told “Closing Bell.”“We don’t like to do that because we disenfranchise customers and we disappoint customers, so we always look at that as a last resort, but that is an option that we will pursue if we need to if the program doesn’t settle down; if we can’t get a good handle on the data and the less data we have, the more risk premium we need to put into our products and that means the prices are higher.”
Obamacare opportunities… for identity theft
POSTED AT 11:31 AM ON FEBRUARY 8, 2014 BY JAZZ SHAW
Jillian Kay Melchior has an informative – and rather alarming – article up at National Review detailing a less discussed aspect of Obamacare which consumers should be aware of. Identity theft gets a lot of coverage in the media (think Target most recently), but I was unaware that the majority of such theft and fraud takes place in the area of medical supplies and services.
Most identity theft in the United States is medical-related, according to a recent report from the Identity Theft Resource Center. The survey was released even as certain aspects of Obamacare enrollment have raised concerns about identity theft and consumer privacy.The Center defines medical identity theft as “the fraudulent use of an individual’s personally identifiable information, such as name, Social Security number, and/or medical insurance identity number to obtain medical goods or services, or to fraudulently bill for medical goods or services using an unlawfully obtained medical identity,” also noting that it “has profound consequences for patients, insurance providers and health care providers.”In 2012 alone, medical identity theft increased by nearly 25 percent, affecting 1.85 million Americans, according to another recent report from the Ponemon Institute, which researches privacy issues.
This makes sense, since it’s probably easier to fraudulently steal a large amount of money from a giant, overburdened medical insurance system than to take a small amount from an individual who may be closely watching their credit card statements each month. It’s a new world of organized crime taking place in cyberspace. And now, consider the “opportunities” opening up to such criminals if there are millions of people feeding their personal information into a new, untested, and highly unstable online system like the healthcare dot gov website. It should give us pause.
But that doesn’t mean that opportunities for the “small business” individual thief are completely absent. The so called “navigators” who are supposed to help you find your way through the byzantine maze of Obamacare have access to all sorts of information which could pave the way to mischief. But they’re all trustworthy, honest individuals, right? Melchior finds that, at least in California, that may not be such a safe assumption either.
At least 43 convicted criminals are working as Obamacare navigators in California, including three individuals with records of significant financial crimes.Although some of the offenses are decades old, and although convicted criminals account for only 1 percent of the 3,729 certified enrollment counselors in the state, Californians still have good cause to be concerned about their privacy…Limited statistics released by Covered California — the state’s new health-insurance exchange — showed that one navigator has repeat forgery offenses — one in 1982, then another in 1994, with a burglary in between. Another had two forgery convictions in 1988, in addition to a domestic-violence charge a decade later. Another committed welfare fraud in 1999 and had shoplifted on at least two prior occasions. Since 2000, individuals now working as navigators have committed crimes including child abuse, battery, petty theft, and evading a police officer. At least seven navigators have multiple convictions.
The sub-title of that second article really says it all. Officials say a criminal record should not keep someone from getting a job. But why this job?
Bad ideas, when crafted into legislation, result in bad laws. Even good ideas, when implemented stupidly, can turn sour quickly. But when you stupidly implement a bad idea, you’ve entered a whole new universe of fail.
2/7/14.....
Shut It Down
DNI, HHS urged to shut Obamacare website until security issues resolved
BY:
President Barack Obama and two senior aides are being urged to suspend all use of the Obamacare computer network until recent U.S. intelligence warnings of potential cyber attacks from Belarus are resolved.
Michele Bachmann (R., Minn.), a member of the House Permanent Select Committee on Intelligence, called for the suspension in letters to the president, Director of National Intelligence James Clapper, and Health and Human Services Secretary Kathleen Sebelius. She warned that “the American people’s personal information submitted to Healthcare.gov could be at risk from cyber attacks across the globe.”
“Intelligence officials reportedly briefed the administration that Healthcare.gov software potentially written by a state-owned firm in Belarus could contain malware and allow surreptitious access to Americans’ health and financial information,” she stated, adding that Belarus is a close ally of Russia.
Bachmann told Clapper that a report posted to the U.S. government’s Open Source Center website had been removed and that the report revealed that Belarusian software engineers were suspected of inserting malicious code in the Obamacare network.
The healthcare network is made up of seven computer hubs that link major federal agencies with some 300 health care providers and insurance firms and some 3 million people who have signed up for health care coverage.
Bachmann reminded Clapper that she had questioned him about the report during an intelligence committee hearing this week.
Clapper stated that he was unaware of the report or its recall.
“However, a DNI spokesman has since confirmed the existence of this report,” she stated in the Feb. 6 letter.
The lawmaker then requested a copy of the report, as well as an explanation of why it was produced and withdrawn from internal circulation.
She then urged Clapper to tell HHS to shut down the Healthcare.gov network until proper security testing is carried out in order to prevent the possible loss of personal data or violations of privacy rights of Americans who used the network.
“Intelligence is on the front lines of ensuring that the American people’s personal information is safe from international cyber threats, and too much is at stake to have so many unanswered questions about Healthcare.gov’s security,” she said.
The healthcare network, one of the president’s most important domestic policy items, has been plagued with problems since it debuted Oct. 1.
Obama told Fox News Channel on Sunday that the software problems, which he described as “glitches,” had been fixed. He made no mention of the potential implanting of malware from Belarus during the pre-Super Bowl interview.
Bachmann, in a separate letter to Sebelius, stated she was concerned that the HHS’ Centers for Medicare and Medicaid Services (CMS), the agency in charge of overseeing Healthcare.gov, could not confirm no malicious software from Belarus is hidden in the software.
“I am writing to respectfully request information on whether or not any code for Healthcare.gov was written in Belarus—or any other country outside the United States—and an explanation of why CMS did not know where all the code was written,” Bachmann said.
“Until these questions are answered and until Healthcare.gov has undergone a proper end-to-end stress test, I urge you to immediately shut down Healthcare.gov so no American’s personal data and privacy rights are jeopardized,” she said.
Copies of the letters were sent to Obama.
Former intelligence officials said the withdrawal of the cyber threat report was an indication of intelligence politicization, a practice barred by regulations for all U.S. intelligence agencies. Politicization occurs when intelligence is skewed or suppressed because it presents unwelcome views or conflicts with administration policies.
A DNI spokesman earlier this week denied the report was withdrawn for political reasons, insisting that it was not properly vetted.
CIA Director John Brennan told the House hearing this week that he was unaware of the report or its withdrawal. The Open Source Center is located at CIA headquarters in Virginia.
DNI spokesman Shawn Turner said Clapper received the letter and “looks forward to providing a timely response.”
The Open Source Center on Jan. 29 distributed a report titled, “United States’ Affordable Care Act Software – Cyber Attack Target.” The report was not coordinated with “subject matter experts, did not meet OSC tradecraft standards, and did not follow established procedures for pre-publication review,” he said.
“The document was recalled for these reasons and because evidence used in the report did not support the title or any conclusion that the software was compromised,” Turner said. “The report will not be reissued.”
The handling of the report was a “rare breakdown” in internal vetting, Turner added. “The cause of the breakdown has been identified and steps are being taken to prevent it from happening again.”
Spokesmen for Sebelius and the White House either had no immediate comment or did not respond to email requests for comment.
The Bachmann letters followed a report in the Washington Free Beacon published Monday revealing that U.S. intelligence agencies early last month discovered information indicating that software developers under Belarus state control had been involved in developing the Obamacare software.
The intelligence was based in part on comments by Belarusian official Valery Tsepkalo who is director of the government-backed High-Technology Park (HTP) in Minsk.
Tsepkalo stated last summer in an interview broadcast on Russian radio that HHS was among his clients and that “we are helping Obama complete his insurance reform.”
“Our programmers wrote the program that appears on the monitors in all hospitals and all insurance companies—they will see the full profile of the given patient,” Tsepkalo said June 25 on Voice of Russia Radio.
Efforts to reach Tsepkalo for comment were unsuccessful.
One U.S. official said: “The U.S. Affordable Care Act software was written in part in Belarus by software developers under state control, and that makes the software a potential target for cyber attacks.”
Concerns about malicious software in the network were compounded by an incident in February 2013 when large segments of U.S. Internet traffic were hijacked to Belarus. Security officials said it was likely the data was sifted for government and economic intelligence before being rerouted back to the United States.
Additionally, the potential for cyber attacks is increased because the Belarusian government is a Soviet-style dictatorship and U.S. adversary.
The potential of Belarus-origin malware, combined with the Internet hijacking of data to Belarus and the hostile Minsk regime, “makes the software written in Belarus a potential target of cyber attacks for identity theft and privacy violations” of Americans, the U.S. official familiar with the report said.
Officials urged HHS to launch security reviews of the network software for malicious code.
All medical facilities and insurance companies in the United States currently use the software.
White House spokeswoman Caitlin Hayden said the warning in the intelligence report prompted a review of Obamacare software but that no links to Belarus or malicious software had been found.
“So far HHS has found no indications that any software was developed in Belarus,” she said. “However, as a matter of due diligence, they will continue to review the supply chain. Supply chain risk is real and it is one of our top concerns in the area of cyber-security.”
Some 55 contractors at a cost of more than $400 million were involved in the development of Healthcare.gov’s software.
2/6/14.....
Obama Considering Three Year Extension To Obamacare
Submitted by Tyler Durden on 02/06/2014 15:37 -0500
While Washington debates over what is the proper explanation of the CBO's report which explicitly states that millions of workers will drop out of the labor force over the next decade thanks to Obamacare, Obama himself may have finally thrown in the towel, realizing that the longer the full implementation of Obamacare is delayed, the longer the myth that it is a viable Ponzi scheme - as opposed to non-viable - can persist. Perhaps this explains why AP reports that the White House is now considering an extension of the president's decision to let people keep their individual insurance policies even if they are not compliant with the health care overhaul, according to two top industry officials.
Avalere Health CEO Dan Mendelson said Thursday that the administration may let policyholders keep that coverage for an additional three years, stressing that no decision has been made. Policymakers are waiting to see what rate hikes health insurers plan for the insurance exchanges that are key to the overhaul's coverage expansions."The administration is entertaining a range of options to ensure that this individual market has stability to it and that would be one thing that they could do," he said.Avalere Health is a market analysis firm, but Mendelson said his company was not advising the administration on exchange policy. He said he has had informal discussions with administration officials about the extension, but he didn't identify them.A spokeswoman for the Department of Health and Human Services, Joanne Peters, said "We are continuing to examine all sorts of ways to provide consumers with more choices and to smooth the transition as we implement the law."
Earlier, Mark Bertolini, Chairman and CEO of Aetna and the nation's third largest insurer, told analysts during his earnings call that he had heard the plans may be extended. Perhaps a more important thing Bertolini said is that his company may pull out of markets if the Medicare cuts are too high, adding that 2015 may be challenging due to medicare cuts. This may have been the final straw that pushed the administration into action.
However, even a longer extension than was rumored previously will hardly help reinstate the policies of all those millions who lost coverage in the lead up to the Obamacare enactment as insurance companies know that terms will once again change eventually, so why go through the headache of temporary reinstatement just to cut all those "non-compliant" individuals once again?
Individual policyholders were hit with a wave of cancellation notices last year because their coverage was less robust than what is required under the law, and many states allowed insurance companies to simply cancel them.The wave of cancellation notices — at least 4.7 million of them — hit just when the new HealthCare.gov website was experiencing some of its worst technical problems, and it undercut the president's well-publicized promise that if you liked your plan you could keep it.
You couldn't.
At first the White House went into damage-control mode, arguing that many of the cancelled plans were "junk" insurance and consumers would be better off with the broader coverage available through the health care law's new insurance markets.But soon Obama was forced to reverse course, urging insurers and state regulators to allow policyholders to keep their existing plans for an additional year. Most states complied with the request.Now the administration is considering adding more years to this extension to avoid another wave of problems if rates on the exchange climb too high and people are left without an affordable coverage option. Health insurers are supposed to submit by May the rates they want to charge on the exchanges next year.
Actually, the only reason why Obama is suddenly willing to compromise over every aspect of his "crowning achievement" is that finally its tactical, and strategic failure has become clear for all to see. So it would be best to enact it piecemeal, and claim success for whatever legacy aspects of the system are working, while blasting everything that his unprecedentedly complicated, centrally-planned contraption has unleashed.
Finally, why three years? Because by then Obama will be gone (absent some very radical changes to presidential term rules), and Obamacare will be someone else's problem.
2/4/14......
http://www.latimes.com/business/la-fi-obamacare-patients-20140205,0,5417742.story#axzz2sQssirFs
After overcoming website glitches and long waits to get Obamacare, some patients are now running into frustrating new roadblocks at the doctor's office.
A month into the most sweeping changes to healthcare in half a century, people are having trouble finding doctors at all, getting faulty information on which ones are covered and receiving little help from insurers swamped by new business.
Experts have warned for months that the logjam was inevitable. But the extent of the problems is taking by surprise many patients — and even doctors — as frustrations mount.
Aliso Viejo resident Danielle Nelson said Anthem Blue Cross promised half a dozen times that her oncologists would be covered under her new policy. She was diagnosed last year with non-Hodgkin's lymphoma and discovered a suspicious lump near her jaw in early January.
But when she went to her oncologist's office, she promptly encountered a bright orange sign saying that Covered California plans are not accepted.
"I'm a complete fan of the Affordable Care Act, but now I can't sleep at night," Nelson said. "I can't imagine this is how President Obama wanted it to happen."
To hold down premiums under the healthcare law, major insurers have sharply cut the number of doctors and hospitals available to patients in the state's new health insurance market.
Now those limited options are becoming clearer, and California officials say they are receiving more consumer complaints about access to medical providers. State lawmakers are also moving swiftly to ease some of the problems that have arisen.
"It's a little early for anyone to know how widespread and deep this problem is," said California Insurance Commissioner Dave Jones. "There are a lot of economic incentives for health insurers to narrow their networks, but if they go too far, people won't have access to care. Network adequacy will be a big issue in 2014."
The latest travails come at a crucial time during the rollout of Obama's signature law. Government exchanges and other supporters of the healthcare law are trying to boost enrollment, particularly among young and healthy people, ahead of a March 31 deadline.
Of course, complaints about outdated provider lists and delays in getting a doctor's appointment were common long before the healthcare law was enacted. But some experts worry the influx of newly insured patients and the cost-cutting strategies of health plans may further strain the system.
Maria Berumen, a tax preparer in Downey, was uninsured for years because of preexisting conditions. The 53-year-old was thrilled to find coverage for herself and her husband for $148 a month after qualifying for a big government subsidy.
She jumped at the chance in early January to visit a primary-care doctor for long-running numbness in her arm and shoulder as a result of bone spurs on her spine. The doctor referred her to a specialist, and problems ensued. At least four doctors wouldn't accept her health plan — even though the state exchange website and her insurer, Health Net Inc., list them as part of her HMO network.
"It's a phantom network," Berumen said.
It was no surprise to her family doctor, Ragaa Iskarous. She has run into this problem repeatedly with other patients in the last month, the doctor said. "This is really driving us crazy."
Berumen said she was seen by a neurosurgeon Thursday — after state regulators intervened on her behalf.
Insurers say they are working hard to resolve customers' problems as they arise, and they continue to add physicians to augment certain geographic areas and medical specialties.
"Any huge implementation like this comes with a lot of moving parts," said Health Net spokesman Brad Kieffer. "There is a learning curve for everyone, and we expect as time goes on these issues should dissipate."
Looking to head off potential problems, government regulators and patient advocates are pushing for tougher rules to ensure health plans provide timely access to care.
Last week, the California Assembly approved legislation enabling people who lost coverage because of the overhaul to keep seeing their doctors if they're pregnant or undergoing treatment for cancer or other conditions.
Nelson, the cancer patient in Orange County, and her family lost their previous coverage when Aetna stopped selling individual policies in the state last year. After numerous complaints to her new insurer, Anthem, and to public officials, the company said it would cover visits to her current oncologist through March 31.
Nelson said such a temporary extension doesn't solve the problem, and as a result, she's rushing to check out other policies for herself before open enrollment closes in March.
A spokesman for Anthem said the company "continually works to update its provider directories to ensure accuracy" and helps customers with these issues on a case-by-case basis.
Nationwide, about 70% of new insurance plans under the healthcare law feature relatively narrow hospital networks compared with many existing plans, according to consulting firm McKinsey & Co.
"It's pretty clear insurers responded to greater competition by trying to hold down costs through narrower networks," said Larry Levitt, senior vice president at the nonprofit Kaiser Family Foundation. "Insurers have made the judgment that people prefer lower premiums to broader networks."
Health policy experts and some consumer advocates say the trade-offs may pay off. Despite some consumer complaints, the exclusion of some higher-priced hospitals such as Cedars-Sinai Medical Center from nearly all exchange plans is a positive sign, they say.
"The Affordable Care Act often gets accused of not doing enough to control costs," said Ian Hill, senior fellow at the Urban Institute, a Washington think tank. "Excluding some of the most expensive hospitals and providers who don't demonstrate high-quality outcomes is one ripple effect that may help."
The Covered California exchange began enrollment in October without the provider directory it had promised. Delays and glitches ensued for weeks, frustrating many consumers who complained that it was impossible to compare health plans without details on what hospitals and doctors were included. In November, the exchange updated its directory.
The exchange said its 11 health plans offer more than 58,000 physicians to choose from, representing 80% to 90% of practicing physicians in the state.
The California Medical Assn. credits the exchange for fixing many of the initial problems but maintains that the state's data are still flawed, often because of incorrect information from health plans. Insurers blame doctor's offices for frequently giving wrong information.
Scott Marshutz of Dana Point said he picked a Blue Shield PPO plan in the exchange so he and his wife would have greater choice of doctors.
But when he booked an appointment recently with his orthopedic surgeon, the doctor's office said it wasn't taking Covered California plans.
http://www.zerohedge.com/news/2014-02-04/obamacare-crush-workforce-25-million-workers-next-decade-cbo-admits
Obamacare To Crush Workforce By 2.5 Million Workers In Next Decade, CBO Admits
Submitted by Tyler Durden on 02/04/2014 11:30 -0500
When the "impartial" Congressional Budget Office first attempted to predict the impact on the US labor force as a result of the administration healthcare ponzi scheme, also known affectionately as Obamacare and less affectionately by other names, it estimated that 800,000 Americans would drop out of the labor force by 2021. Moments ago it just revised that projection, admitting that it was off by the usual 100% or so: the hit to the US labor force due to Obamacare is now estimated to soar to 2.3 million through 2021, and furthermore the CBO just admitted that the enrollment rate will be dramatically below the White House's baseline estimates, with 2 million fewer people signing up this year than previously estimated.
In brief, as the CBO admits (before it is forced to adversely reduce the numbers once more) the law will lead to 2 million fewer workers in 2017, 2.3 million in 2021 and 2.5 million through 2024. This represents a 1.5% to 2.0% reduction in the numbers of hours worked. As the WSJ recalls, CBO last year projected 7 million people would enroll for health insurance through health care exchanges in 2014, but Tuesday it said technical problems that plagued the program's rollout forced it to lower its estimate by 1 million people.
"Those changes primarily reflect the significant technical problems that have been encountered in the initial phases of implementing the [law]," the CBO said. It said it couldn't yet revise estimates for future years. CBO also projected 8 million new people would qualify for Medicaid and other expanded coverage this year, down from a 2013 estimate of 9 million people.
The health care law's open enrollment process began in October and runs through March, and CBO estimated "the number of [people who sign up [for coverage] will increase sharply toward the end of the period." Or not.
And here it is straight from the horse's mouth:
The ACA’s largest impact on labor markets will probably occur after 2016, once its major provisions have taken full effect and overall economic output nears its maximum sustainable level. CBO estimates that the ACA will reduce the total number of hours worked, on net, by about 1.5 percent to 2.0 percent during the period from 2017 to 2024, almost entirely because workers will choose to supply less labor—given the new taxes and other incentives they will face and the financial benefits some will receive.
What does that mean?It means this: "reduced incentives to work attributable to the Affordable Care Act (ACA)—with most of the impact arising from new subsidies for health insurance purchased through exchanges—will have a larger negative effect on participation toward the end of that period." Just don't call it a welfare program.
The above in numbers:
The reduction in CBO’s projections of hours worked represents a decline in the number of full-time-equivalent workers of about 2.0 million in 2017, rising to about 2.5 million in 2024. Although CBO projects that total employment (and compensation) will increase over the coming decade, that increase will be smaller than it would have been in the absence of the ACA....The number of people who will receive exchange subsidies—and who thus will face an implicit tax from the phaseout of those subsidies that discourages them from working—will be smaller initially than it will be in later years. The number of enrollees (workers and their dependents) purchasing their own coverage through the exchanges is projected to rise from about 6 million in 2014 to about 25 million in 2017 and later years, and most of those enrollees will receive subsidies. Although the number of people who will be eligible for exchange subsidies is similar from year to year, workers who are eligible but do not enroll may either be unaware of their eligibility or be unaffected by it and thus are unlikely to change their supply of labor in response to the availability of those subsidies.
The CBO's mea culpa:
CBO’s estimate that the ACA will reduce aggregate labor compensation in the economy by about 1 percent over the 2017–2024 period—compared with what would have occurred in the absence of the act—is substantially larger than the estimate the agency issued in August 2010. At that time, CBO estimated that, once it was fully implemented, the ACA would reduce the use of labor by about one-half of a percent. That measure of labor use was calculated in dollar terms, representing the change in aggregate labor compensation that would result. Thus it can be compared with the reduction in aggregate compensation that CBO now estimates to result from the act (rather than with the projected decline in the number of hours worked).CBO’s updated estimate of the decrease in hours worked translates to a reduction in full-time-equivalent employment of about 2.0 million in 2017, rising to about 2.5 million in 2024, compared with what would have occurred in the absence of the ACA. Previously, the agency estimated that if the ACA did not affect the average number of hours worked per employed person, it would reduce household employment in 2021 by about 800,000.25 By way of comparison, CBO’s current estimate for 2021 is a reduction in full-time-equivalent employment of about 2.3 million.
If you like your horrible 2010 forecast, you can keep your horrible 2010 forecast.
As for the most recent one, which too will be the source of comedy in one year's time, here it is (link).
Great news: ObamaCare website written by Belarus-linked programmers
POSTED AT 12:01 PM ON FEBRUARY 4, 2014 BY ED MORRISSEY
Don’t worry. I have it on good authority from a Nigerian prince and a friend who lost his wallet in Vladivostok that these guys were totally on the level:
U.S. intelligence agencies last week urged the Obama administration to check its new healthcare network for malicious software after learning that developers linked to the Belarus government helped produce the website, raising fresh concerns that private data posted by millions of Americans will be compromised.The intelligence agencies notified the Department of Health and Human Services, the agency in charge of the Healthcare.gov network, about their concerns last week. Specifically, officials warned that programmers in Belarus, a former Soviet republic closely allied with Russia, were suspected of inserting malicious code that could be used for cyber attacks, according to U.S. officials familiar with the concerns.The software links the millions of Americans who signed up for Obamacare to the federal government and more than 300 medical institutions and healthcare providers.“The U.S. Affordable Care Act software was written in part in Belarus by software developers under state control, and that makes the software a potential target for cyber attacks,” one official said.
We’ve been hearing all along that the architecture of the Healthcare.gov website is particularly susceptible to hacker penetration. David Kennedy, a former Marine Corps cyberwarfare expert turned Internet security consultant, has warned since October that the system leaves critical identity information exposed. That got worse rather than better after the operational fixes made in November, and HHS doesn’t even have systems in place to detect such intrusions.
Small wonder why the Obama administration didn’t want to brief Congress on security issuesin December. These security gaps were presumed to be the product of incompetent programming and management. Until now, we didn’t realize that the subcontracts for programming went in part to a firm connected with a hostile regime. Belarus has remained a satellite to Moscow with a dictator in charge ever since the breakup of the Soviet Union, Alexander Lukashenko, and the regime is decidedly unfriendly to the West. Currently, the US doesn’t even recognize the legitimacy of Lukashenko’s government after his rigged 2010 election.
How did this happen? Normally, we’d pay good money to keep hostile regimes from penetrating our government operations. In this case, it looks as though we paid them to do it. Great job, HHS!
But it’s not all bad. If you think your identity information has been hijacked, just call the ObamaCare hotline. Be sure to ask for Peggy.
2/3/14....
Videos: Mayo Clinic employees get benefit cuts, cost hikes after ObamaCare
POSTED AT 2:01 PM ON FEBRUARY 3, 2014 BY ED MORRISSEY
And needless to say, they’re not happy about it. The premiere health-care provider network and big Minnesota employer will have to cut benefits for its own employees, in part to comply with ObamaCare’s coverage mandates and in part to deal with exploding insurance premiums under the new law. First came the announcement last Friday that the changes would hit in 2015, after the employer mandates kick into force, KTTC reported:
The CEO of Mayo Clinics tried to explain why this was necessary, but any economist could explain that much. When you penalize so-called “Cadillac” health plans and force insurers to absorb more risk, coverage will get reduced and prices will go up:
“For folks that use no medical care beyond primary care visits and preventative services, their premiums could go down, or stay the same,” Nesse said. “But folks who need more care will be responsible for more of the cost of that care.”That’s bad news for folks who have diseases like diabetes.We could not find any Mayo employee willing to speak on camera, but one who spoke with us anonymously says the cost of his insulin copay has more than doubled just this year.He says he and other diabetic Mayo retirees have had to stop taking some of their medication. He fears the changes in 2015 will make it even more expensive.
We’ve featured a lot of videos of people discovering just how much disruption ObamaCare has caused, but this has another aspect to it. The others talk about rising costs now, but this one shows that companies have already begun planning for the employer mandate that takes effect in January 2015. The White House put off enforcement of that part of ObamaCare until mid-November, which would put it past the midterms, but that’s not going to fool anyone. Businesses seeing the impact of current disruptions and the mandate’s enforcement will start adapting long before the due date. Mayo is just getting way ahead of the curve; many employers will wait until late summer to roll out these changes and price hikes, or announce that they’re dropping coverage altogether and sending their employees into the ObamaCare exchanges.
That’s going to make a lot of people angry — just as they prepare to walk into the voting booths.
Thousands of ObamaCare site error appeals reportedly going unfixed
FoxNews.com
Thousands of people who tried to sign up for a health plan via the federal healthcare exchange website, Healthcare.gov, have seen their appeals to fix site issues go unanswered.
The Washington Post, citing internal government data, reports that approximately 22,000 Americans have filed appeals to try and get site errors corrected. The complaints range from being denied coverage altogether to being overcharged for coverage to being steered into the wrong program.
So far, months after the site launched October 1, the appeals have been untouched. What's more, the Post reports, people who have tried to call the marketplace directly for assistance, have been told that the Healthcare.gov computer system is not yet allowing workers to correct enrollment records.
In theory, error appeals can be filed through the site itself, by phone, or by mail. However, only the mail appeal is currently available. But according to the Post, the appeal by mail process only goes as far as scanning the seven-page forms and transferring them to a computer system, where they currently sit unread and uncorrected.
A CMS spokesman told the Post "We are working to fully implement the appeals system." In the meantime, the paper reported, applicants are being told to go back to Healthcare.gov and start over, thought it is not clear how many of the 22,000 who complained of errors have done so.
However, the lack of action on appeals means that some who signed up for plans taking effect January 1 have been stuck with health plans costing them too much. One of those, 27-year-old West Virginian Addie Wilson, told the Post she was paying $100 more per month than necessary for her insurance, with a deductible that's $4,000 too high.
ObamaCare sticker shock: Don’t forget the deductibles
POSTED AT 1:21 PM ON FEBRUARY 3, 2014 BY ERIKA JOHNSEN
As ever, the fact that health insurers have been hiking up the prices of deductibles as one avenue through which they can help absorb the heightened costs of ObamaCare is not news to anyone who’s been paying attention — which is why a new study pointing to comparable premiums between ObamaCare-offered policies and employer-based policies doesn’t quite paint the whole picture of the law’s effects. Via the Fiscal Times:
According to a report released by PwC’s Health Research Institute, insurance premiums on the new health exchanges are cheaper than those paid by the majority of Americans who have employer-based coverage—partly because of high deductibles.The report found that the average cost of premiums sold on the Obamacare exchanges is about $5,844 annually —or 4 percent less than the average cost of $6,119 for an employer-provided plan with comparable benefits. …Still, PwC’s study doesn’t account for other costs to consumers—like deductibles, which are likely to be more expensive under the new plans. A study by HealthPocket Inc. in December found that the average individual deductible for Obamacare’s bronze plan was $5,081 a year—42 percent higher than the average deductible of $3,589 for an individually purchased plan.“Picking one dimension as PwC and others do gives a distorted picture of what the consumer is likely to experience,” Joe Antos, health policy analyst at the conservative American Enterprise Institute said. He added that the PwC study also doesn’t mention other changes that affect consumers like insurers narrowing provider access.
Consumers in areas like, say, rural Georgia, where both skyrocketing premiums and heightened deductibles mean that health insurance is making less and less economic sense for a whole slew of people, via WaPo:
If Lee Mullins lived in Pittsburgh, he could buy mid-level health coverage for his family for $940 a month. If he lived in Beverly Hills, he would pay $1,405.But Mullins, who builds custom swimming pools, lives in southwest Georgia. Here, a similar health plan for his family of four costs $2,654 a month. …All the dynamics that drive up health costs have coalesced here in southwestern Georgia, pushing up premiums. Expensive chronic conditions such as obesity and cancer are common among the quarter million people in this region. One hospital system dominates the area, leaving little competition. Only one insurer is offering policies in the online marketplace, and many physicians are not participating, limiting consumer choice. …Even some people who qualify for federal assistance, such as Stacie Brown, owner of a pottery shop, are balking. The cheapest “bronze” plan for Brown, her husband and son would cost the family $300 a month but not begin paying medical bills until they exceeded the $6,300 individual deductible.
Ouch.
2/2/14......
Sunday, February 02, 2014 12:00 PM
Real Life Obamacare Small Business, Benefit-Shifting Example
Here is an interesting video regarding the effects of Obamacare on all the employees at at Simonetta's auto repair shop in Pennsylvania. The video was made by a local TV station.
A couple premiums dropped, but most went up, some by huge amounts. In every case deductibles soared. Every person involved is worse off than before.
Link if video does not play: Employees in Pennsylvania Company Learn of Increased Health Costs Due to Obamacare
Partial Transcript
Jeff and Dave used to have a $1,250 deductible. Since Obamacare went into effect, it's now jumped 60 percent to $2,000. That's nothing compared to Brian, Kristi, and Judy who have kids. they are going to pay twice that, four grand."
"I don't know how President Obama thinks he's helping us because we can't afford this, we can't afford to pay these co-pays, to pay these deductibles on what we're making," says one of the workers.
Another worker adds, "They call it the affordable health plan. There's nothing affordable about it. I can't afford it."
Winners and Losers
Obamacare shifted the winners and losers.
A small number of people gained big (those with no insurance, those with preexisting conditions, and those who get free Medicaid). To pay for that, a large number of people lost, to varying degrees.
Mike "Mish" Shedlock
A couple premiums dropped, but most went up, some by huge amounts. In every case deductibles soared. Every person involved is worse off than before.
Link if video does not play: Employees in Pennsylvania Company Learn of Increased Health Costs Due to Obamacare
Partial Transcript
Jeff and Dave used to have a $1,250 deductible. Since Obamacare went into effect, it's now jumped 60 percent to $2,000. That's nothing compared to Brian, Kristi, and Judy who have kids. they are going to pay twice that, four grand."
"I don't know how President Obama thinks he's helping us because we can't afford this, we can't afford to pay these co-pays, to pay these deductibles on what we're making," says one of the workers.
Another worker adds, "They call it the affordable health plan. There's nothing affordable about it. I can't afford it."
Winners and Losers
Obamacare shifted the winners and losers.
A small number of people gained big (those with no insurance, those with preexisting conditions, and those who get free Medicaid). To pay for that, a large number of people lost, to varying degrees.
Mike "Mish" Shedlock
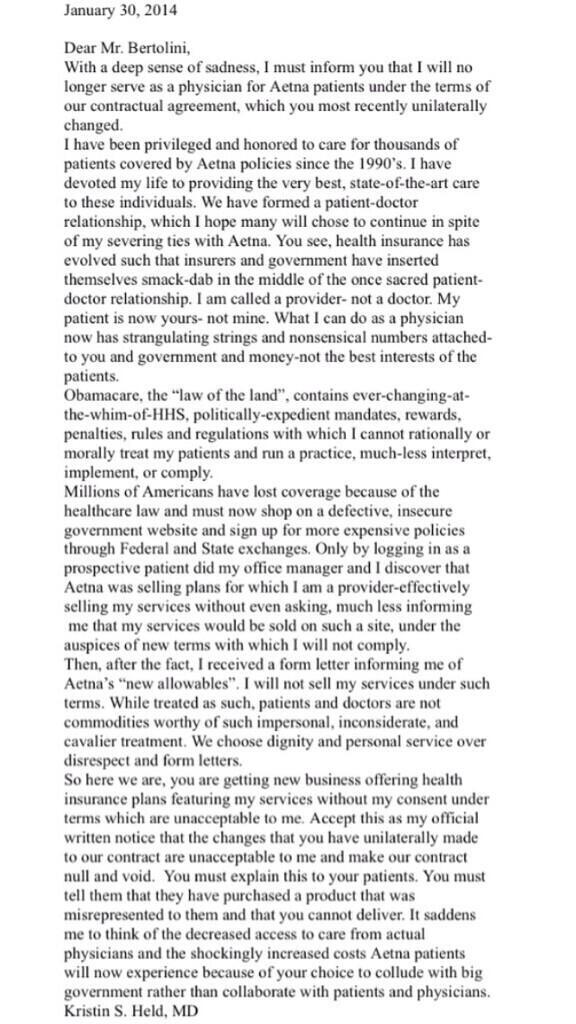
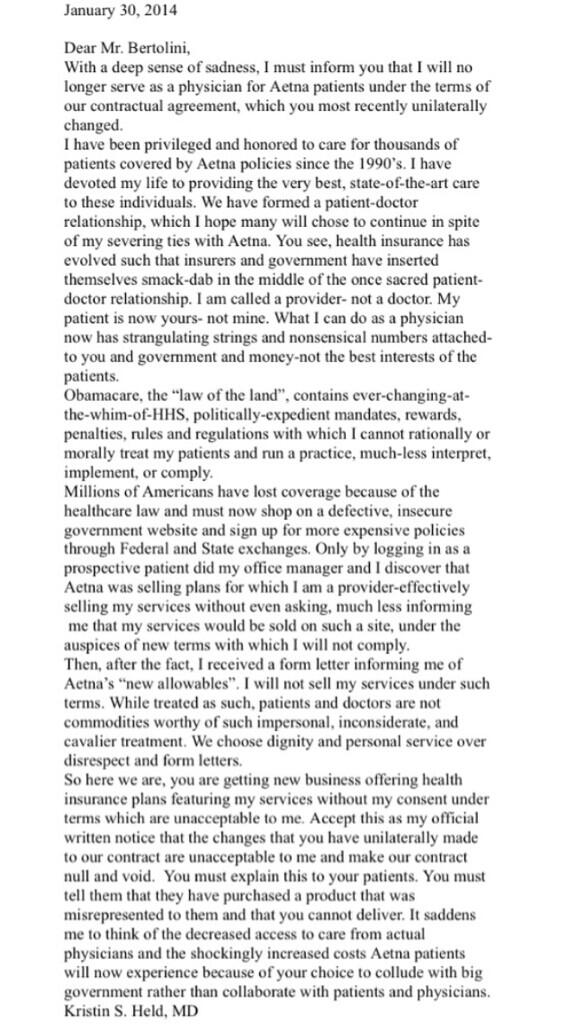
Kris Held is a doctor “on a mission to get government out of medicine.” Here’s part of her bio:
I have read The Patient Protection and Affordable Care Act (Obamacare), tweeted it and studied it. I will not implement, comply with it or let my patients live or die by it. Co-Founder AmericanDoctors4Truth.org
And she meant every word.
Here’s the letter she sent to Aetna when she discovered the insurer was “selling plans for which I am a provider-effectively selling my services without even asking, much less informing me that my services would be sold on such a site, under the auspices of new terms with which I will not comply.”
Here’s what happened when Held sent her letter.
Pelosi: ObamaCare incompetence “not my responsibility”
POSTED AT 10:01 AM ON JANUARY 31, 2014 BY ED MORRISSEY
This appearance by Nancy Pelosi on The Daily Show starts to run off the rails almost immediately. Jon Stewart starts off by asking Pelosi about why people talk about politics rather than policy, to which Pelosi answers by … complaining about Republicans. Stewart doesn’t take the bait, though, and starts pressing Pelosi for answers as to why big-government politicians can’t produce competent government — and gets stunned by her admission that she can’t explain why ObamaCare failed:
Stewart said that Democrats are then required to make a stronger case. He said that Democratic governance now appears “chaotic” and their execution of legislation appears to “lack efficiency.” When Pelosi again blamed Republicans for this condition, Stewart became even more agitated.When he asked why it was so difficult to get a company to execute the Affordable Care Act’s insurance exchange website “competently,” Pelosi replied, “I don’t know.”“What do you mean you don’t know? How do you not know?” Stewart asked laughing.
To which Nancy Pelosi responded: “It’s not my responsibility.” Hmmm. Who ran the House when the ObamaCare bill passed, with only votes from her party? Who claimed at the time that we couldn’t know how awesome this bill would be until it passed, because you couldn’t expect politicians to actually read a 2800-page bill before they voted on it? Given that this passed entirely on votes from her own party, and with some procedural chicanery thrown in for good measure, does she feel no responsibility at all for the results of this legislation she herself championed?
That’s a pretty good answer to Stewart’s broader point. He cites the ongoing problems at the VA as evidence that there is “clearly something systemic” in government incompetence:
“Do we have a foundational problem? Is there a corruption in the system that needs to be addressed?” Stewart asked. Pelosi went on to detail the issues with bureaucracy and the failure of departments to communicate with each other. “Okay, do something about it,” Pelosi said.“I was actually going to say that to you,” Stewart interjected.
The systemic problem is the fact that big-government regimes like ObamaCare won’t work because central planning of large economies never work, for reasons laid out by economist F. A. Hayek decades ago in The Road to Serfdom. History has only proven Hayek correct over and over again, while utopians keep insisting that the problem is just the people involved in its implementation. And Hayek predicts why incompetents and bullies end up at the top of those systems, too. Maybe Stewart should read it. It’s far too late for Pelosi.
Update: Here’s a rebuttal from someone who doesn’t grasp the difference between ObamaCare and, say, SNAP or Social Security:
From Road to Serfdom, pages 148-149:There is no reason why in a society which has reached the general level of wealth which ours has attained the first kind of security should not be guaranteed to all without endangering general freedom. …. [T]here can be no doubt that some minimum of food, shelter, and clothing, sufficient to preserve health and the capacity to work, can be assured to everybody. … Nor is there any reason why the state should not assist the individual in providing for those common hazards of life against which, because of their uncertainty, few individuals can make adequate provision.”Where, as in the case of sickness and accident, neither the desire to avoid such calamities nor the efforts to overcome their consequences are as a rule weakened by the provision of assistance – where, in short, we deal with genuinely insurable risks – the case for the state’s helping to organize a comprehensive system of social insurance is very strong. There are many points of detail where those wishing to preserve the competitive system and those wishing to super-cede it by something different will disagree on the details of such schemes; and it is possible under the name of social insurance to introduce measures which tend to make competition more or less ineffective. But there is no incompatibility in principle between the state’s providing greater security in this way and the preservation of individual freedom.The product of approximately 30 seconds of Google searching. You should issue a correction for misrepresenting Hayek’s work. But you won’t. You won’t respond to my email to explain why you won’t issue a correction either. You aren’t interested in being right, only in winning. But feel free to prove me wrong on any of these counts.
Of course I’m aware of this passage. I don’t disagree with it, either; I’m not a Randian. But the key difference is that social-insurance programs like SNAP don’t impose top-down control over the economy or a significant part of it. ObamaCare explicitly does do that by issuing mandates for coverage, mandates on employers, and mandates on people to buy it. Central control over this economy is its main purpose. SNAP, Medicaid, and even Medicare (in principle) don’t force everyone under the rubric of that control, either; there is no “grocery insurance” mandate, as an example. They are voluntary programs which allow for people to choose entry or refuse it for the regular marketplace. ObamaCare controls exert force universally in the health-care market, thanks to its mandates.
Just as Hayek argued, when government takes top-down control of economies, they remove choice, innovation, and get things incredibly wrong — because central controllers cannot possibly know the proper choices in the millions and billions of transactions in those economies. Innovation dies quickly, especially when people try to work around it to actually have their needs met, and it gets more dysfunctional rather than less. Furthermore, the dysfunction and failures in the system will always get blamed on lack of cooperation, resulting in escalating punishments and intrusion – and more arbitrariness in following the law, which we’re already seeing. The people getting rewarded in those systems end up being the people more willing to abuse power in order to achieve the political ends of the top-down central controllers — and become less and less accountable as that process moves forward.
This is what happens when one Googles for excerpts rather than reading and comprehending the entire work. It reminds me of people who Google Bible verses to use in arguments with no comprehension of their meaning.
Worker says hours cut due to Obamacare; Obama cites as reason minimum wage has to increase
 |
**Written by Doug Powers
During a “Google Hangout” on Friday, President Obama heard from somebody who said he was a fry cook who’s had his hours cut from full time so the place he works could “avoid paying health care” (presumably due to Obamacare regs). President Obama’s answer? That’s why we have to raise the minimum wage.
This exchange takes place at about the 14 minute mark of the video below (partial transcript):
Question: Good afternooon, Mr. President. My name is Darnell Summers, I’m 57 years old, and I work in the fast food industry. I have been on strike four times — I’m only making $7.25 an hour — I’ve been on strike four times in association with Wisconsin Jobs Now to try to get a increase in wages and a fast food union, with no prevail. My question to you is, what can you and Congress do, to help people as myself, in this situation … survive. Because with $7.25 — and we were broken down to part time to avoid paying health insurance — we can’t survive. It’s not living.Obama: Well, Darnell, I agree with you. And on Tuesday in my State of the Union I talked about this. We’ve got to make sure the economy is growing and creating jobs. We gotta make sure folks have the skills to get those jobs. But we’ve also got to make sure that work pays. And the minimum wage in this country has not gone up in a very long time. It’s actually worth about 20 percent less than when Ronald Reagan came into office back in 1980. And, I think, the one thing Americans agree on is that if you work full time in this country you should not be in poverty when you’re raising your family.
Because 40 hours a week at $7.25 an hour is so much worse than 28 hours a week at $10.10?
If raising the minimum wage to offset the hour cuts and other hits to the economy Obamacare hath wrought, pretty soon the minimum wage is going to be $25 an hour and they’ll still be pretending not to know why so many people remain worse off than ever.
A different questioner had this hard-hitting
“Hello, Mr President, this is about the coolest thing ever,” he said, explaining that “out of a million [questions] that I’d love to ask you over a beer somewhere,” one stood out:One man to another, one father to another, one American to another… How are you? … Is everything good with you, man?Obama laughed. “We should have that beer, because that might take a longer answer,” he said.
I assume NBC News signed him to a contract shortly after the Hangout ended.




Solar activity jolts Equador and Indo volcanos,southern hemisphere's atmosphere loaded up with particulates :
ReplyDeletehttp://www.weather.com/maps/maptype/satelliteworld/southamericasatellite_large_animated.html
Indo's volcano's ash has gone up over Himilayas and will track east over China,Japan,into pacific jetstream over Alaska through Canada to the Great Lakes area and beyond to dump more Fukmeshima fallout snow on top of all the contaminated snow acumulation on N America..
http://www.weather.com/maps/maptype/satelliteworld/westpacificglobalsatellite_large_animated.html
Solar flares will increase later this month as Mercury rotates closer.
NW